ESHO
European Society of Hyperthermic
Oncology
Biological effects of hyperthermia
The overall aim to study the biological effects of hyperthermia is to better understand the effectiveness of the treatment (science-based medicine) and to improve its use (treatment optimisation). The studies on hyperthermic effects encompass both in vitro molecular cell biological and in vivo animal studies.
Although many of the above-mentioned is still in experimental phase or sometimes even only explored at the level of fundamental research, they have provided guidelines for improved clinical use of hyperthermia and will likely do so in the future.
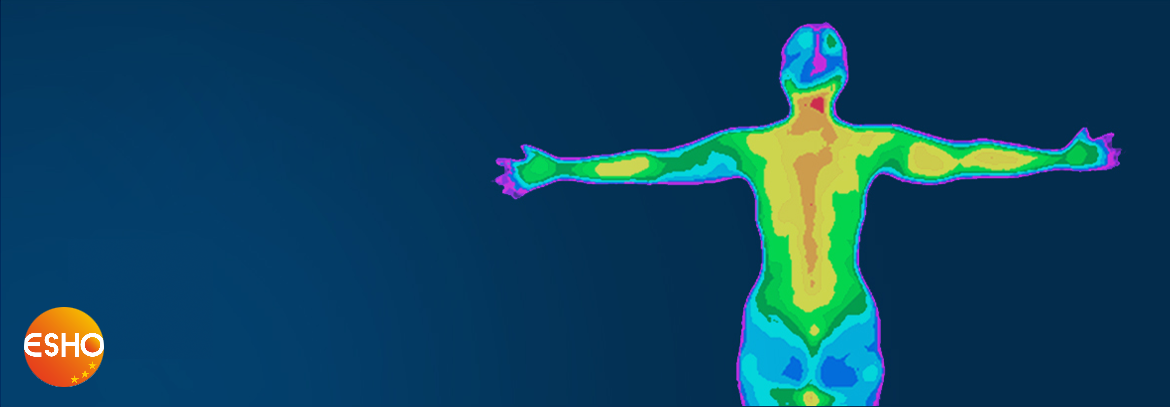
When cells are heated beyond their normal growth temperature, they can die from this treatment. Those cells that survive the heat treatment can become sensitised to radiation and to a number of chemotherapeutic agents (see figure 1).
Whereas tumour cells per se are generally not more sensitive to these effects of hyperthermia than normal cells, the physiology of the tumour cell (low pH, poor nutrient status) makes it more susceptible to heating. Moreover, because the vascularisation of tumours is often chaotic, blood flow-related cooling during heating of tumours is less than in normal tissue, meaning that the actual temperature rise obtained by the external heating devises (see physics) can be higher than in the surrounding normal tissue. So, the cellular effects of hyperthermia as such, combined with the selectivity towards tumours due to physiology, have provided a scientific basis to use hyperthermia as an effective adjuvant in cancer therapy.
Heat and radiation
Until so far, the cellular studies on hyperthermia have focussed on molecular mechanisms of cellular heat sensitivity, transient heat resistance (thermotolerance), heat and radiation interaction and heat and drug interaction. The studies have revealed that the predominant consequence of hyperthermia is that proteins unfold and can aggregate (see figure 2). By this, myriads of processes in the cell are disturbed and can lead to cell death directly. For heat and radiation interaction, it was shown that radiation does not enhance the effects of heat, but rather that heat enhances the effects of radiation. It was found that - likely due to protein denaturation - heat retards the repair of radiation-induced DNA damage, leaving more damage unrepaired and hence causing more cells to die from the radiation injury. Importantly, the synergy between radiation and heat is highly dependent on the order of application and highest when given simultaneously.
Heat and drugs
In the case of heat and drug interaction, the situation is more complex as drugs metabolism is usually complex, requiring multiple steps. E.g., the powerful anti-cancer drug cis-platin first has to traverse the plasma membrane and escape from intracellular detoxification and drug-export pumps before it can damage its target, the DNA, in the cell nucleus. And even than, cells can repair this DNA damage and survive. So, the net-effect of a drug depends on the sum of these individual steps. As hyperthermia leads to a rather general (i.e. non-specific) denaturation of proteins in the cells, it may interfere with any of the steps in the drug toxicity process. Indeed, this has been proven to be the case. In fact, a well-known characteristic in chemotherapy is the development of chemoresistance. This resistance is usually multi-factorial involving up-regulation in one or more steps of the cellular drug-defence mechanisms. The finding that hyperthermia by its global effect can affect each of these steps makes it a potential treatment to counteract this drug-resistance phenotype. For some drugs, like the platinum compounds, this hypothesis was confirmed, showing that hyperthermia can make resistant cells platinum-responsive again. The systemic character of chemotherapy, in contrast to the more locally applied heat shock, may be the primary reason that combined chemotherapy-hyperthermia protocols have not been explored very extensively in the clinic. The current development and exploration of novel devices for whole body hyperthermia may revive this type of research.
Thermotolerance
A disadvantage intrinsically associated with hyperthermia is that one heat treatment can cause a transient resistant against a subsequent treatment (thermotolerance).
In radiotherapy, a standard treatment regimen consists of a 6 weeks course of radiation doses, given each Monday to Friday. If one would like to apply hyperthermia with each of these radiation treatments, this thermotolerance would certainly negatively interfere with the effectiveness of the treatment. Therefore, the mechanism underlying thermotolerance are extensively explored to find ways to minimise its development. It is clear now that so-called Heat Shock Proteins play a central role in thermotolerance, and therefore their function and regulation is been studied in several laboratories. Besides being involved in thermotolerance, these proteins may play important roles in tumour immunity and resistance to cell death stimuli (apoptosis) in general.
Tumour physiology
Besides these cellular features, tumour physiology, tumour blood flow and blood vessel permeability are important aspects of thermobiology. Besides the above mentioned effects of these issues on the selective heat sensitivity of tumour cells, poor tumour blood flow is an important aspect causing radiation resistance since poor tumour vascularisation is associated with poor oxygenation and cells lacking oxygen are radioresistant. Due to the general vasodilatation effect of elevated temperature, heat may reoxygenate tumours making them more sensitive to radiation again. Finally, due to heating blood vessel wall permeability can increase, which may result in better drug delivery to tumours, especially when these drugs are enclosed in so-called thermosensitive liposomes that only release their drug content when encountering a heated (tumour) area.